
Healthy Living – Regular Check-Ups are Important

Start your year off right by scheduling your annual checkup. Regular health exams and tests can help find problems before they start. They also can help find problems early, when your chances for treatment and cure are better. By getting the right health services, screenings, and treatments, you are taking steps that help your chances for living a longer, healthier life. Your age, health and family history, lifestyle choices (i.e. what you eat, how active you are, whether you smoke), and other important factors impact what and how often you need healthcare
Recommended Health Services
[vc_tta_accordion]Screening means checking your body for cancer before you have symptoms. Getting screening tests regularly may find breast and cervical cancers early, when treatment is likely to work best.
Breast Cancer
Breast cancer is sometimes found after symptoms appear, but many women with breast cancer have no symptoms. This is why regular breast cancer screening is so important. Breast cancer screening means checking a woman’s breasts for cancer before there are signs or symptoms of the disease. Although breast cancer screening cannot prevent breast cancer, it can help find breast cancer early, when it is easier to treat. Talk to your doctor about which breast cancer screening tests are right for you, and when you should have them.
Cervical Cancer
The cervix is the lower part of the uterus, the place where a baby grows during pregnancy. Cancer screening is looking for cancer before you have any symptoms. Cancer found early may be easier to treat.
Cervical cancer screening is usually part of a woman’s health checkup. There are two types of tests: the Pap test and the HPV test. For both, the doctor or nurse collects cells from the surface of the cervix. With the Pap test, the lab checks the sample for cancer cells or abnormal cells that could become cancer later. With the HPV test, the lab checks for HPV infection. HPV is a virus that spreads through sexual contact. It can sometimes lead to cancer. If your screening tests are abnormal, your doctor may do more tests, such as a biopsy.
If you have a low income or do not have health insurance, you may be able to get a free or low-cost screening test through the National Breast and Cervical Cancer Early Detection Program. Find out if you qualify.
What Is Colorectal Cancer Screening?
A screening test is used to look for a disease when a person doesn’t have symptoms. (When a person has symptoms, diagnostic tests are used to find out the cause of the symptoms.)
Colorectal cancer almost always develops from precancerous polyps (abnormal growths) in the colon or rectum. Screening tests can find precancerous polyps, so that they can be removed before they turn into cancer. Screening tests can also find colorectal cancer early, when treatment works best.
When Should I Begin to Get Screened?
You should begin screening for colorectal cancer soon after turning 50, then continue getting screened at regular intervals. However, you may need to be tested earlier than 50, or more often than other people, if—
- You or a close relative have had colorectal polyps or colorectal cancer.
- You have an inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
- You have a genetic syndrome such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (Lynch syndrome).
If you think you are at increased risk for colorectal cancer, speak with your doctor about—
- When to begin screening.
- Which test is right for you.
- How often to get tested.

Nearly 1 in 3 American adults has high cholesterol. Too much cholesterol puts you at risk for heart disease and stroke, two leading causes of death in the United States. High cholesterol has no signs or symptoms, so the only way to know if you have it is to get your cholesterol checked.
Who Needs to Get Their Cholesterol Checked?
- Most healthy adults should have their cholesterol checked every 4 to 6 years.
- Some people, such as people who have heart disease or diabetes or who have a family history of high cholesterol, need to get their cholesterol checked more often.
- Children and adolescents should have their cholesterol checked at least once between ages 9 and 11 and again between ages 17 and 21.
Talk to your health care team about your health history and how often you need to have your cholesterol checked.
What Happens During a Cholesterol Test?
The cholesterol test, or screening, requires a simple blood draw. You may need to fast (not eat or drink) for 8 to 12 hours before your cholesterol test. Be sure to ask your doctor how to prepare for the test.
The cholesterol test checks your levels of:
- Low-density lipoprotein (LDL) or “bad” cholesterol. Having high levels of LDL cholesterol can lead to plaque buildup in your arteries and result in heart disease or stroke.
- High-density lipoprotein (HDL) or “good” cholesterol. HDL is known as “good” cholesterol because high levels can lower your risk of heart disease and stroke.
- Triglycerides, a type of fat in your blood that your body uses for energy. The combination of high levels of triglycerides with low HDL cholesterol or high LDL cholesterol levels can increase your risk for heart attack and stroke.
- Total cholesterol, the total amount of cholesterol in your blood based on your HDL, LDL, and triglycerides numbers.
High blood pressure is a common and dangerous condition. Having high blood pressure means the pressure of the blood in your blood vessels is higher than it should be. About 1 of 3 U.S. adults—or about 75 million people—have high blood pressure. Only about half (54%) of these people have their high blood pressure under control. Many youth are also being diagnosed with high blood pressure. This common condition increases the risk for heart disease and stroke, two of the leading causes of death for Americans. High blood pressure is called the “silent killer” because it often has no warning signs or symptoms, and many people do not know they have it. That’s why it is important to check your blood pressure regularly.
Oral health affects our ability to speak, smile, eat, and show emotions. It also affects self-esteem, school performance, and attendance at work and school. Oral diseases—which range from cavities to gum disease to oral cancer—cause pain and disability for millions of Americans.
Oral health problems in adults include the following:
- Untreated tooth decay. More than 1 in 4 (26%) adults in the United States have untreated tooth decay.
- Gum disease. Nearly half (46%) of all adults aged 30 years or older show signs of gum disease; severe gum disease affects about 9% of adults.
- Tooth loss. Complete tooth loss among adults aged 65-74 years has steadily declined over time, but disparities exist among some population groups.5 If left untreated, cavities (tooth decay) and periodontal (gum) disease lead to tooth loss.
- Oral cancer. Oral cancers are most common in older adults, particularly in people older than 55 years who smoke and are heavy drinkers.
- People treated for cancer who have chemotherapy may suffer from oral problems such as painful mouth ulcers, impaired taste, and dry mouth.
- Chronic diseases. Having a chronic disease, such as arthritis, heart disease or stroke, diabetes, emphysema, hepatitis C, a liver condition, or being obese may increase an individual’s risk of having missing teeth and poor oral health.
- Patients with weakened immune systems, such as those infected with HIV and other medical conditions (organ transplants) and who use some medications (e.g., steroids) are at higher risk for some oral problems.
- Chronic disabling diseases such as jaw joint diseases (TMD), autoimmune conditions such as Sjögren’s Syndrome, and osteoporosis affect millions of Americans and compromise oral health and functioning, more often among women.
Visit the dentist regularly. Checkups can find tooth decay, gum disease, and other problems before they lead to more serious issues.
The goal of screening for prostate cancer is to find cancers that may be at high risk for spreading if not treated, and to find them early before they spread. There is no standard test to screen for prostate cancer. Two tests that are commonly used to screen for prostate cancer are:
- Prostate Specific Antigen (PSA) Test
- Digital Rectal Examination (DRE)
Who should get screened for prostate cancer:
In 2018, the U.S. Preventive Services Task Force (USPSTF) made the following recommendations about prostate cancer screening
- Men who are 55 to 69 years old should make individual decisions about being screened for prostate cancer with a prostate specific antigen (PSA) test.
- Before making a decision, men should talk to their doctor about the benefits and harms of screening for prostate cancer, including the benefits and harms of other tests and treatment.
- Men who are 70 years old and older should not be screened for prostate cancer routinely.
This recommendation applies to men who—
- Are at average risk for prostate cancer.
- Are at increased risk for prostate cancer.
- Do not have symptoms of prostate cancer.
- Have never been diagnosed with prostate cancer.
Other organizations, like the American Urological Association, the American Cancer Society, and the American College of Physicians may have other recommendations
Talk to Your Doctor
If you are thinking about being screened, you and your doctor should consider—
- If you have a family history of prostate cancer.
- If you are African-American.
- If you have other medical conditions that may make it difficult for you to be treated for prostate cancer if it is found, or that may make you less likely to benefit from screening.
- How you value the potential benefits and harms of screening, diagnosis, and treatment.
Skin cancer is the most common form of cancer in the United States. The two most common types of skin cancer—basal cell and squamous cell carcinomas—are highly curable, but can be disfiguring and costly to treat. Melanoma, the third most common skin cancer, is more dangerous and causes the most deaths. The majority of cases of these three types of skin cancer are caused by overexposure to ultraviolet (UV) light.
Anyone can get skin cancer, but people with certain characteristics are at greater risk—
- A lighter natural skin color.
- Skin that burns, freckles, reddens easily, or becomes painful in the sun.
- Blue or green eyes.
- Blond or red hair.
- Certain types and a large number of moles.
- A family history of skin cancer.
- A personal history of skin cancer.
Report any unusual moles or changes in your skin to your doctor. Also talk to your doctor if you are at increased risk of skin cancer.
CDC recommends everyone between the ages of 13 and 64 get tested for HIV at least once.
People at higher risk should get tested more often. If you were HIV-negative the last time you were tested, the test was more than one year ago, and you can answer yes to any of the following questions, then you should get an HIV test as soon as possible:
- Are you a man who has had sex with another man?
- Have you had sex—anal or vaginal—with a partner who has HIV?
- Have you had more than one sex partner since your last HIV test?
- Have you injected drugs and shared needles, syringes, or other drug injection equipment (for example, cookers) with others?
- Have you exchanged sex for drugs or money?
- Have you been diagnosed with or treated for another sexually transmitted disease?
- Have you been diagnosed with or treated for hepatitis or tuberculosis (TB)?
- Have you had sex with someone who could answer yes to any of the above questions or someone whose sexual history you don’t know?
You should be tested at least once a year if you keep doing any of these things. Sexually active gay and bisexual men may benefit from more frequent testing (for example, every 3 to 6 months).
If you’re pregnant, talk to your health care provider about getting tested for HIV and other ways to protect you and your child from getting HIV.
Before having sex for the first time with a new partner, you and your partner should talk about your sexual and drug-use history, disclose your HIV status, and consider getting tested for HIV and learning the results.
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C.
Who should be tested?
Hepatitis A
Testing for hepatitis A is not routinely recommended.
Hepatitis B
CDC recommends hepatitis B testing for:
- People born in countries with 2% or higher HBV prevalence
- Men who have sex with men
- People who inject drugs
- People with HIV
- Household and sexual contacts of people with hepatitis B
- People requiring immunosuppressive therapy
- People with end-stage renal disease (including hemodialysis patients)
- People with hepatitis
- People with elevated ALT levels
- Pregnant women
- Infants born to HBV-infected mothers
Hepatitis C
CDC recommends hepatitis C testing for:
- Current or former injection drug users, including those who injected only once many years ago
- Everyone born from 1945 to 1965
- Anyone who received clotting factor concentrates made before 1987
- Recipients of blood transfusions or solid organ transplants before July 1992
- Long-term hemodialysis patients
- People with known exposures to hepatitis C virus, such as health care workers or public safety workers after needle sticks involving blood from someone infected with hepatitis C virus and recipients of blood or organs from a donor who tested positive for the hepatitis C virus
- People with HIV
- Children born to mothers with hepatitis C
The U.S. Preventive Services Task Force recommends hepatitis C testing for additional groups including:
- People in jails or prisons
- People who use drugs snorted through the nose (in addition to people who inject drugs)
- People who get an unregulated tattoo
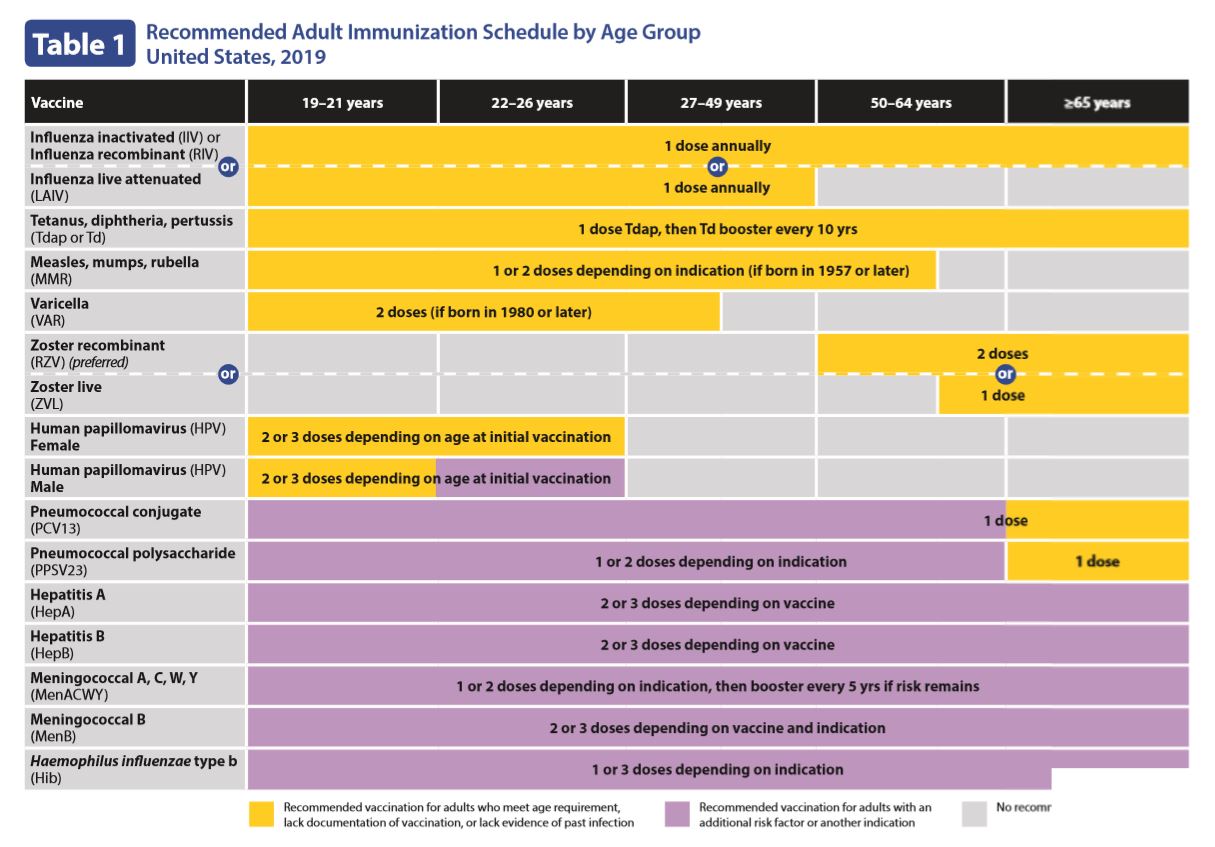
Recommended Adult Immunization for ages 19 years or older, United States, 2019
- Haemophilus influenzae type b vaccination
- Hepatitis A vaccination
- Hepatitis B vaccination
- Human papillomavirus vaccination
- Influenza vaccination
- Measles, mumps, and rubella vaccination
- Meningococcal vaccination
- Pneumococcal vaccination
- Tetanus, diphtheria, and pertussis vaccination
- Varicella vaccination
- Zoster vaccination
The best place to go for health services is your regular health care provider. However, if you do not have one, the links below provide other options.
- CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) offers free or low-cost mammograms and Pap tests. Find out if you qualify.
- HIV Testing Resources
- Find Affordable Health Care in Your Community (HRSA)
Source:
- CDC
- US National Library of Medicine


Most Commented