
UTERINE CANCER

Uterine cancer is one of the few cancers with increasing incidence and mortality in the United States, reflecting, in part, increases in the prevalence of overweight and obesity since the 1980s. It is the fourth most common cancer diagnosed and the seventh most common cause of cancer death among U.S. women.
What is uterine cancer?
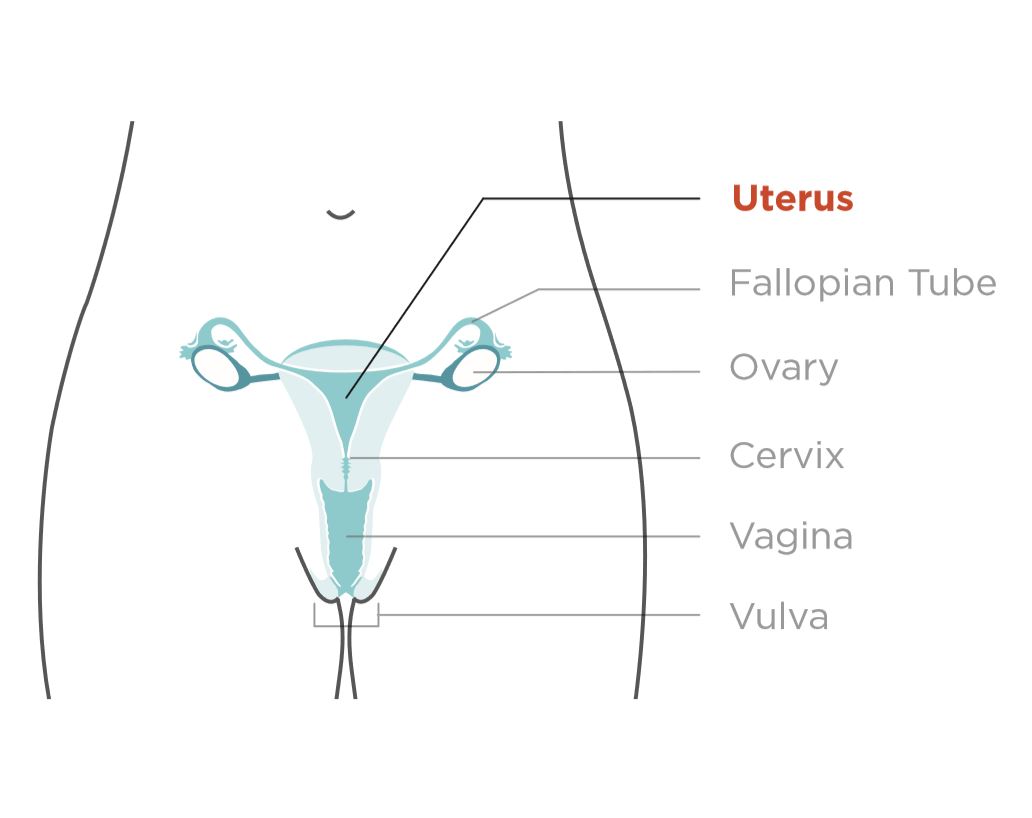
When cancer starts in the uterus, it is called uterine cancer. The uterus is the pear-shaped organ in a woman’s pelvis. Also called the womb, the uterus is where the baby grows when a woman is pregnant.
There are two main types of uterine cancer:
Endometrial cancer: The most common type of uterine cancer. Endometrial cancer forms in the lining of the uterus, which is called the endometrium.
Uterine sarcoma: A rare type of uterine cancer that forms in the muscle or other tissue of the uterus. When uterine cancer is found early, treatment is most effective.
Who gets uterine cancer?
All women—except those whose uterus was removed by having a hysterectomy—are at risk for uterine cancer, and the risk increases with age. Most uterine cancers are found in women who are going through or have gone through menopause. Each year, approximately 50,600 women in the United States get uterine cancer.
What are the signs and symptoms of uterine cancer?
Signs and symptoms of uterine cancer include:
- Vaginal discharge that is not normal for you.
- Abnormal vaginal bleeding. The bleeding may be abnormal because of how heavy it is or when it happens, such as bleeding after you have gone through menopause; bleeding between periods; or any other bleeding that is longer or heavier than normal for you.
- Pain or pressure in your pelvis. Pay attention to your body, and know what is normal for you. If you have vaginal bleeding that is not normal for you, see a doctor right away.
If you have any of the other signs and they last for two weeks or longer, see a doctor. These things may be caused by something other than cancer, but the only way to know is to see a doctor.
What raises a woman’s chance of getting uterine cancer?
There is no way to know who will get uterine cancer. However, several factors may increase the chance that you will get uterine cancer, including if you:
- Are older than age 50.
- Are obese (having a high, unhealthy amount of body fat).
- Take estrogen by itself for hormone replacement during menopause. In general, when estrogen is used, it should be in combination with the other female hormone, progesterone.
- Have had trouble getting pregnant, or have had fewer than five periods in a year at any time in your life before starting menopause.
- Take tamoxifen, a drug used to prevent or treat certain types of breast cancer.
- Have people in your family with a history of uterine, colon, or ovarian cancer.
If one or more of these is true for you, it does not mean you will get uterine cancer, but you should talk with a doctor to see if he or she recommends more frequent exams. Women who have an inherited form of colorectal cancer, called hereditary nonpolyposis colorectal cancer syndrome, have an increased risk of getting uterine cancer.
This may be true for you if you have close female relatives (i.e., your mother, grandmother, sister, aunt, or daughter) who have had uterine or ovarian cancer. If so, talk to a doctor about having annual exams and endometrial biopsies, starting at age 35.
How can I help prevent or lower my chance of getting uterine cancer?
There is no known way to prevent uterine cancer. But these things may reduce your chance of getting uterine cancer:
- Using birth control pills.
- Maintaining a healthy weight and being physically active.
- Taking progesterone if you are taking estrogen.
Are there ways to find uterine cancer early?
There are no simple and reliable ways to test for uterine cancer in women who do not have any signs or symptoms. The Pap test does not screen for uterine cancer. The only cancer the Pap test screens for is cervical cancer. This is why it is important to know the signs and symptoms of uterine cancer and to see a doctor if you have any of them.
If you have symptoms or are at high risk for uterine cancer, your doctor may perform an endometrial biopsy or a transvaginal ultrasound. These tests can be used to help diagnose or rule out uterine cancer. Your doctor may do these tests in his or her office, or may refer you to another doctor. The doctor might perform more tests if the endometrial biopsy does not provide enough information, or if symptoms continue.
How Is Uterine Cancer Treated?
If your doctor says that you have uterine cancer, ask to be referred to a gynecologic oncologist—a doctor who has been trained to treat cancers like this. This doctor will work with you to create a treatment plan.
Types of Treatment
Uterine cancer is treated in several ways. It depends on the kind of uterine cancer and how far it has spread. Treatments include surgery, chemotherapy, and/or radiation.
- Surgery: Doctors remove cancer tissue in an operation.
- Radiation: Using high-energy rays (similar to X-rays) to kill the cancer.
- Hormone Therapy: Hormone therapy removes hormones or blocks their action and stops cancer cells from growing. Hormones are substances made by glands in the body and circulated in the bloodstream.
- Chemotherapy: Using special medicines to shrink or kill the cancer. The drugs can be pills you take or medicines given in your veins, or sometimes both.
Different treatments may be provided by different doctors on your medical team.
- Gynecologic oncologists are doctors who have been trained to treat cancers of a woman’s reproductive system.
- Surgeons are doctors who perform operations.
- Medical oncologists are doctors who treat cancer with medicine.
- Radiation oncologists are doctors who treat cancer with radiation.
Visit the National Cancer Institute for more information about treatments for the most common kinds of uterine cancer: endometrial cancer and uterine sarcoma.
Source:
- CDC
Graphic:
- CDC


Most Commented