
ovarian cancer awareness month
According to CDC Each year, about 20,000 women in the United States get ovarian cancer. Ovarian cancer causes more deaths than any other cancer of the female reproductive system (Gynecologic cancer), but it accounts for only about 3% of all cancers in women.
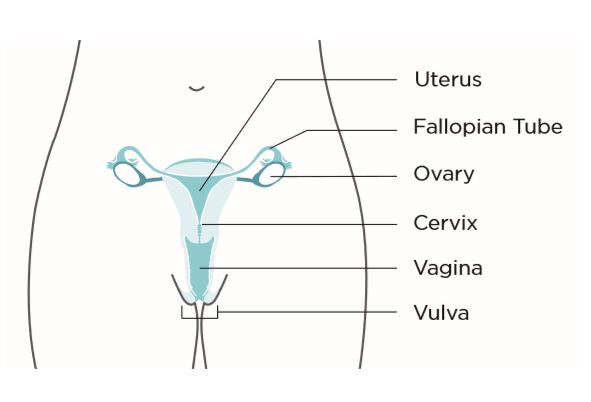
There are five main types of cancer that starts in a woman’s reproductive organs, cervical, ovarian, uterine, vaginal, and vulvar. A sixth type of gynecologic cancer is the very rare fallopian tube cancer.
Of all the gynecologic cancers, only cervical cancer has a screening test—the Pap test—that can find this cancer early, when treatment can be most effective. Since there is no simple and reliable way to screen for any gynecologic cancers except cervical cancer, it is especially important to recognize warning signs, and learn if there are things you can do to reduce your risk.
What is Ovarian cancer?
When cancer starts in the ovaries or in the related areas of the fallopian tubes and the peritoneum, it is called ovarian cancer.
Women have two ovaries that are located in the pelvis, one on each side of the uterus. The ovaries make female hormones and produce eggs. The fallopian tubes are long, slender tubes, one on each side of the uterus. Eggs pass from the ovaries through the fallopian tubes to the uterus. The peritoneum is the tissue lining that covers organs in the abdomen.
Who gets ovarian cancer?
All women are at risk for ovarian cancer, but older women are more likely to get the disease than younger women. About 90 percent of women who get ovarian cancer are older than 40. The greatest number of ovarian cancers occurs in women aged 60 years or older. Women who have had both ovaries removed have a much lower risk of ovarian cancer. Each year, approximately 21,000 women in the United States get ovarian cancer and about 14,000 die from it.
What are the signs and symptoms of ovarian cancer?
Ovarian cancer may cause the following signs and symptoms:
• Vaginal bleeding (particularly if you are past menopause) or discharge from your vagina that is not normal for you.
• Pain or pressure in the pelvic area.
• Abdominal or back pain.
• Bloating.
• Feeling full too quickly or difficulty eating.
• A change in bathroom habits, such as more frequent or urgent need to urinate and or constipation.
Pay attention to your body and know what is normal for you. If you have unusual vaginal bleeding, see a doctor right away. If you have any of the other signs for two weeks or longer and they are not normal for you, see a doctor. They may be caused by something other than cancer, but the only way to know is to see a doctor.
What raises a woman’s chance of getting ovarian cancer?
There is no way to know if you will get ovarian cancer. However, there are several factors that may increase your risk, including if you:
• Are middle aged or older.
• Have close family members (such as your mother, sister, aunt, or grandmother) on either your mother’s or father’s side, who have had ovarian cancer.
• Have had breast, uterine, or colorectal cancer.
• Have an Eastern European (Ashkenazi) Jewish background.
• Have never given birth or have had trouble getting pregnant.
• Have endometriosis (a condition where tissue from the lining of the uterus grows elsewhere in the body).
• Have tested positive for a genetic abnormality called BRCA1 or BRCA2, or one associated with Lynch syndrome. In addition, some studies suggest that women who take estrogen by itself (estrogen without progesterone) for 10 or more years may have an increased risk of ovarian cancer. If one or more of these is true for you, it does not mean you will get ovarian cancer. But you should talk to a doctor about your risk.
Should I have a genetic test for ovarian cancer?
If you or your family have a history of breast or ovarian cancer, your doctor may recommend genetic testing and counseling. Genetic testing is useful for a very small percentage of women who have a family history of cancer. It is not recommended for all women, but it is important for all women to know their family history.
Genetic testing can help some women find out if they have an increased chance of developing breast and ovarian cancer. It works by finding changes or alterations in genes known as breast cancer susceptibility genes 1 and 2 (BRCA1 and BRCA2). If you are considering genetic testing, you should get genetic counseling to help you decide whether to get tested, and to learn what the test results may mean for you.
Is genetic testing right for you?
If the following is true for you, you may benefit from genetic counseling and testing:
You have an Eastern European (Ashkenazi) Jewish background and on your mother’s or father’s side you have one of the following:
• A first degree relative (i.e., parent, sibling, or child) with breast or ovarian cancer.
• Two second-degree relatives (grandparent, grandchild, uncle, aunt, nephew, niece, or halfsibling) on the same side of the family with breast or ovarian cancer.
You do not have an Eastern European (Ashkenazi) Jewish background, but on your mother’s or father’s side you have one of the following:
• Two first-degree relatives (i.e., parent, sibling, or child) with breast cancer and at least one of them was diagnosed at or before the age of 50.
• A combination of three or more first-or second degree relatives with breast cancer, regardless of the age they were when the cancer was diagnosed.
• A combination of breast and ovarian cancer among first-or-second-degree relatives.
• A first-degree relative with breast cancer in both breasts.
• A combination of two or more first-or-second degree relatives with ovarian cancer, regardless of the age they were when the cancer was diagnosed.
• A first-or-second-degree relative with both breast and ovarian cancer, diagnosed at any age. • A history of breast cancer in a male relative.
How Is Ovarian Cancer Treated?
If your doctor says that you have ovarian, fallopian tube, or primary peritoneal cancers, ask to be referred to a gynecologic oncologist—a doctor who was trained to treat cancers of a woman’s reproductive system. Gynecologic oncologists can perform surgery on and give chemotherapy (medicine) to women with ovarian cancer. Your doctor can work with you to create a treatment plan.
Types of Treatment
Treatment for ovarian cancer usually involves a combination of surgery and chemotherapy.
Surgery: Doctors remove cancer tissue in an operation.
Chemotherapy: Using special medicines to shrink or kill the cancer. The drugs can be pills you take or medicines given in your veins, or sometimes both.
Different treatments may be provided by different doctors on your medical team.
Gynecologic oncologists are doctors who have been trained to treat cancers of a woman’s reproductive system. They perform surgery and give chemotherapy (medicine).
Surgeons are doctors who perform operations.
Medical oncologists are doctors who treat cancer with medicine (chemotherapy).


Most Commented